Low Back Pain and the Brain
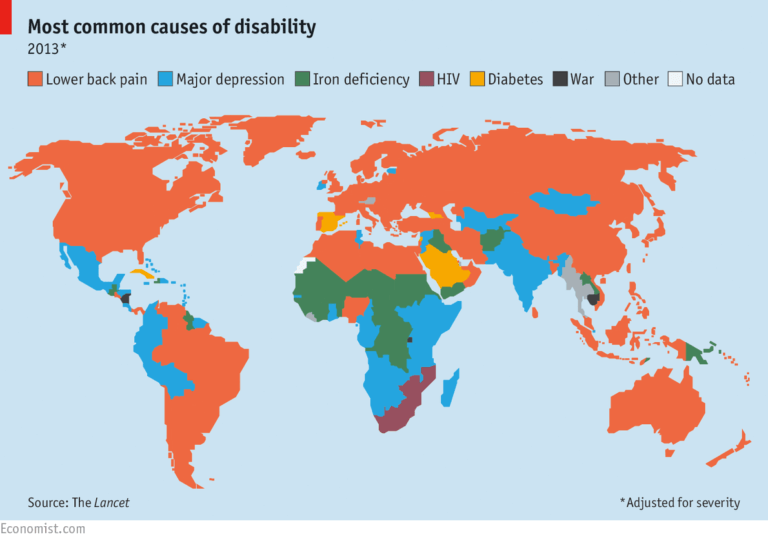
This article is for everyone, as unfortunately 80% of us will at one time get an episode of Low Back Pain (LBP). LBP absolutely plagues this country, as it is the #1 cause of disability for individuals <45 years old and has been labeled “the most debilitating disorder in the western world”. One would think that the heart or the brain would be the most common cause of disability, but not here. Healthcare has a serious issue treating low back pain, especially with the active individual or athlete.
Low Back Pain Statistics: A Snapshot
Figure 1: Most common causes of disability in the world
It is estimated that LBP will become persistent between 10-40% of individuals, aka almost half the individuals who end up having an episode of LBP have their symptoms persist for longer than 3 months. If you are reading this article it is unlikely that your pain has only lasted a couple months. It is probably something you are searching answers for and that it has bothered you for quite some time, maybe 6 months, a year, a couple years, a decade? Unfortunately, you are not the only one.
Low Back Pain (CLBP) is the 3rd highest cause of healthcare spending in the US at 87.6 Billion annually. Americans are out there hurting and are desperately trying to find a solution to their back pain. The traditional model of treating the lumbar spine has failed in being effective at addressing people’s pain and is costly not only to the client but to all of us with copays and deductibles skyrocketing over the last couple years. I am sure the high cost of LBP has contributed to it. (https://www.choosept.com/didyouknow/detail/low-back-neck-pain-cost-americans-billions-in-heal)
So Where Does It All Go Wrong?
Why do so many people who have LBP end up not being able to return to normalcy, or their sport? It’s because the system is broken. It’s 2020 and with all the amazing advances in technology and accessibility with we still have individuals doing one of four things:
Self diagnosing themselves online from Dr. Google which leads to always worst case scenario of either never ending pain or eventual death by a rare disease only seen on House.
The most traditional route: End up going to a physician (which usually takes time to schedule) then referred out to orthopedist (more time to schedule) then receive medical imaging (even more time to schedule), then schedule a follow up (yup you guessed it more time) to find out that you got “junk in trunk” with findings on imaging that seem extremely scary (degenerative) but in all likelihood were probably there well before your symptoms/injury and they didn’t cause a thing. At this point you probably have received ineffective medications, possibly injections, and maybe even a surgical consult. And then maybe you are prescribed PT!
Feel that they cannot be helped: “it’s not that bad, so I will deal with it. So what if I can only deadlift half of what I used to with pain? I’ll live.”
End up going to the most convenient (cheapest, most local) physical therapy office where no one explains what is going on, they are passed to an aide/tech and receive passive treatments (heat, ice, stim, ultrasound) and do nothing to help them progress to their activities or sports and assume this is what “physical therapy is.”
Easy to see where we go wrong. We now know from research that individuals who receive PT care early require less time/sessions for symptom elimination and overall less costs. So, one of our biggest factors is a delay in active treatment such as good quality rehab.
Figure 2: Evidence showing how early adherent (stick to the plan) physical therapy results in less injections, surgeries, # of rehab sessions, and overall money spent.
LBP/Brain Connection
How we treat LBP is the next factor. As mentioned before, medications, injections, surgeries and passive treatments have been proven to not be effective for LBP. Yet these are still the interventions most individuals receive. And this leads to the actual theme of this blog.
Why is this blog called Low Back Pain and The Brain? Because our current research has found that our low back pain is extremely multifactorial. Your back pain is not solely caused by what was found on your X-ray/MRI (Lumbar stenosis, Degenerative Disc Disease, Disc Bulging/Herniations, Spondylosis/spondylolisthesis, Nerve Impingement etc) or perceived “damages” to it.
How Stress can Affect your Pain
We now know that any type of pain (acute/chronic) anywhere on the body (knee, ankle, hip, back etc) has a massive influence from non-pathoanatomical factors such as stress factors (finances, work, failed treatment, what you read online, family, explanations from others, etc) sleep, nutrition, depression, and anxiety.
Have you ever had the moment where your back was killing you and the only thing that was different was that you were stressed out? Maybe from school, relationship, work, or recent scares of an economic recession and virus outbreak? Stress of any sort affects your physiology (your hormones, nerves, and everything in between) and those changes can affect how you feel. Increased tissue tension, less “happy hormones”, decreased joint fluidity/mobility, decreased confidence, poor sleep/recovery and the list goes on and on. Add all that to a lingering issue and we have the recipe for chronic and persistent pain.
We also know that previous memories and histories of pain affect us today. Hurt your back trying to hit a deadlifting PR? Well now every time you come near any sort of deadlifting or hell lifting motion from the ground, your brain (always wanting to protect the host aka you) will link that lovely activity to be a threat because of the past. And guess what, when the brain perceives something as threat, do you think it’s going to allow you to do it smoothly? Not a chance. Once again, your physiology will be taken for a whirl (in a bad way) and make that lift a million times harder than it needs to be. You are essentially fighting against yourself, without you even knowing it.
The Next Step
So, most of you would think why don’t I say a couple positive affirmations about previous harmful activity, and I will be good to go? I completely encourage that behavior, and wish it were that easy (for some it may very well be that easy). For the others, it requires more finesse. Addressing what may be over-exerting the back during the activity (poor balance between the posterior chain, core, mobility, etc), chipping away in a graded manner (body weight to kettlebell to barbell) and addressing the stress x-factors may be necessary. The key is to not give up! You are not broken, you just need some guidance in showing that whatever activity is limiting is not a threat.
What we know now is at least more promising than it was when I first started in this profession. Most of the time LBP is benign (not harmful in nature). Yes, despite all that “junk in trunk” or “wear and tear” you found out about from an X-ray in the 90’s, its most likely not the end of the world for you. In fact, there is strong evidence to support that imaging for non-traumatic LBP leads to poorer outcomes (aka longer duration of symptoms, more medical costs, not achieving full resolution of symptoms).
“Imaging findings of spine degeneration are present in high proportions of asymptomatic individuals, increasing with age. Many imaging-based degenerative features are likely part of normal aging and unassociated with pain.”
Fig 3: Age-specific prevalence estimates of “degenerative” spine imaging findings in ASYMPTOMATICpatients. Fig 4: MRI of client treated at Trifecta with “massive L5-S1 disc herniation” who achieved full resolution of symptoms and return to sport (powerlifting) pain free wuthout the need of opiods, injections or surgery
Now this article was definitely targeting individuals with low back pain, but the same “x-factors” that impact LBP can be involved in any neuromusculoskeletal pain. Your shoulder that bothers you every time you try to do a snatch that did not go quite so great a year ago? Or your neck pain that comes around finals season? Or how about your knee pain when you go up the stairs at work? All these have the same factors as we discussed before. And the way to resolve them is similar as well.
So what do we do in a nutshell;
First thing first: biggest advice is to stay active (halted an activity/activities never really did anything for anyone)
Reassurance: You are going to be ok and make it through this
GET immediate/EARLY treatment (specific towards your needs)
No imaging unless red flags (suspicious findings)
AVOID extended rest and time off work
Over the counter medications as needed and directed (consult a physician or pharmacist for this)
Superficial heat (do not rely on this but can be helpful)
Mobilizations/Manipulations
Progressive guided return to your normal daily activities (work, sport, play)
Hope this helps some people out there that have given up hope on their back (or anywhere else). Do not give up, seek help from someone who is trained not only to break down your physical limitations or your form but also address the x-factors that may not seem so obvious. Feel free to contact us anytime, regardless of where you are in the world. Nothing makes us happier to see/hear someone getting back to what they love to do whether it is through us or someone else. We are all on the same team of getting you better!
Dr. Jeremy Boyd aka The Decent Doctor
Feature Image courtesy of https://unsplash.com/@alinnnaaaa
References:
1. O’Sullivan, DipPhysio, PGradDipMThPhD, FACP P, Lin, BSc(Physio), MManipTher, PhD. Acute low back pain: Beyond drug therapies. Pain Manag Today. 2014;1(1):8-13.
2. Hashmi JA, Baliki MN, Huang L, et al. Shape shifting pain: chronification of back pain shifts brain representation from nociceptive to emotional circuits. Brain. 2013;136(9):2751-2768. doi:10.1093/brain/awt211.
3. Moseley GL, Butler DS. Fifteen Years of Explaining Pain: The Past, Present, and Future. J Pain. 2015;16(9):807-813. doi:10.1016/j.jpain.2015.05.005.
4. Nijs J, Paul van Wilgen C, Van Oosterwijck J, van Ittersum M, Meeus M. How to explain central sensitization to patients with “unexplained” chronic musculoskeletal pain: Practice guidelines. Man Ther. 2011;16(5):413-418. doi:10.1016/j.math.2011.04.005.
5. Louw A, Zimney K, O’Hotto C, Hilton S. The clinical application of teaching people about pain. Physiother Theory Pract. 2016;32(5):385-395. doi:10.1080/09593985.2016.1194652.
6. Louw A, Diener I, Butler DS, Puentedura EJ. The Effect of Neuroscience Education on Pain, Disability, Anxiety, and Stress in Chronic Musculoskeletal Pain. Arch Phys Med Rehabil. 2011;92(12):2041-2056. doi:10.1016/j.apmr.2011.07.198.
7. Louw A, Zimney K, Puentedura EJ, Diener I. The efficacy of pain neuroscience education on musculoskeletal pain: A systematic review of the literature. Physiother Theory Pract. 2016;32(5):332-355. doi:10.1080/09593985.2016.1194646.
8. Pires D, Cruz EB, Caeiro C. Aquatic exercise and pain neurophysiology education versus aquatic exercise alone for patients with chronic low back pain: a randomized controlled trial. Clin Rehabil. 2015;29(6):538-547. doi:10.1177/0269215514549033.
9. Brinjikji W, et al. Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. Am J Neuroradiol. 2015;36:811–816. doi: 10.3174/ajnr.A4173.
Are you interested in our services at Trifecta Therapeutics, but live too far away from our facility? Schedule a telehealth visit!